Creatinine
From Wikipedia, the free encyclopedia
| This article needs additional citations for verification. Please help improve this article by adding reliable references. Unsourced material may be challenged and removed. (March 2007) |
| Creatinine | |
|---|---|
 | |
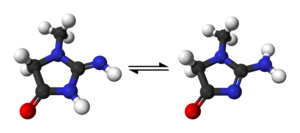 | |
| IUPAC name | 2-amino-1-methyl-5H-imidazol-4-one |
| Identifiers | |
| CAS number | [60-27-5] |
| PubChem | 588 |
| MeSH | Creatinine |
| SMILES | CN1CC(=O)N=C1N |
| Properties | |
| Molecular formula | C4H7N3O |
| Molar mass | 113.118 |
| Appearance | Solid |
| Density | 1.09 g/cm3 |
| Melting point | 300 °C |
| Hazards | |
| NFPA 704 | |
| S-phrases | S24/25 |
| Except where noted otherwise, data are given for materials in their standard state (at 25 °C, 100 kPa) Infobox disclaimer and references | |
Creatinine is a break-down product of creatine phosphate in muscle, and is usually produced at a fairly constant rate by the body (depending on muscle mass).
Contents[hide] |
[edit] Physiology
Creatinine is mainly filtered by the kidney, though a small amount is actively secreted. There is little-to-no tubular reabsorption of creatinine. If the filtering of the kidney is deficient, blood levels rise. As a result, creatinine levels in blood and urine may be used to calculate the creatinine clearance(ClCr), which reflects the glomerular filtration rate (GFR). The GFR is clinically important because it is a measurement of renal function. However, in cases of severe renal dysfunction, the creatinine clearance rate will be "overestimated" because the active secretion of creatinine will account for a larger fraction of the total creatinine cleared. Ketoacids, cimetidine and trimethoprim reduce creatinine tubular secretion and therefore increase the accuracy of the GFR estimate, particularly in severe renal dysfunction. (In the absence of secretion, creatinine behaves like inulin.) A more complete estimation of renal function can be made when interpreting the blood (plasma) concentration of creatinine along with that of urea. In the USA, urea concentration is given as blood urea nitrogen, in mg/In other countries, including those of Europe, urea concentration is measured and quoted in mmol/L. BUN-to-creatinine ratio; ratio of urea to creatinine can indicate other problems besides those intrinsic to the kidney for example, a urea level raised out of proportion to the creatinine may indicate a pre-renal problem such as dehydration. Men tend to have higher levels of creatinine because they have more skeletal muscle than women. Vegetarians tend to have lower creatinine levels, because vegetables contain no creatinine.
[edit] Diagnostic use
Measuring serum creatinine is a simple test and it is the most commonly used indicator of renal function. A rise in blood creatinine levels is observed only with marked damage to functioning nephrons. Therefore, this test is not suitable for detecting early stage kidney disease. A better estimation of kidney function is given by the creatinine clearance test. Creatinine clearance can be accurately calculated using serum creatinine concentration and some or all of the following variables: sex, age, weight, and race as suggested by the American Diabetes Association without a 24 hour urine collection.[1] Some laboratories will calculate the ClCr if written on the pathology request form; and, the necessary age, sex, and weight are included in the patient information.
[edit] Interpretation
In the United States, creatinine is typically reported in mg/dL, while in Canada and Europe μmol/litre may be used. 1 mg/dL of creatinine is 88.4 μmol/l.
The typical reference ranges are 0.5 to 1.0 mg/dL (about 45-90 μmol/l) for women and 0.7 to 1.2 mg/dL (60-110 μmol/l) for men. While a baseline serum creatinine of 2.0 mg/dL (150 μmol/l) may indicate normal kidney function in a male body builder, a serum creatinine of 0.7 mg/dL (60 μmol/l) can indicate significant renal disease in a frail old woman.
More important than absolute creatinine level is the trend of serum creatinine levels over time.
Creatinine levels may increase when ACE inhibitors (ACEI) or angiotensin-II receptor blockers (ARBs) are used in the treatment of chronic heart failure (CHF). Using both ACEI & ARB concomitantly will increase creatinine levels to a greater degree than either of the two drugs would individually. An increase of <30% is to be expected with ACEI or ARB use.
[edit] CT Scans
The creatinine level is usually measured before performing a contrast-enhanced Computed tomography (CT) scan. In a small proportion of patients the administration of iodine based contrast can cause kidney damage. This may be more likely or severe in patients with an elevated baseline serum creatinine level and, again, in rare cases may require temporary or permanent dialysis. The risk can be reduced somewhat in higher-risk patients by choosing a low-osmolality contrast medium.
[edit] See also
- Cystatin C - novel marker of kidney function.
- Creatinine clearance
[edit] References
- ^ Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T (2005). "Diabetic nephropathy: diagnosis, prevention, and treatment". Diabetes Care 28 (1): 164-76. PMID 15616252.
